JAMA: Low-income families with high cost-share levels most likely to forego a child's asthma treatment
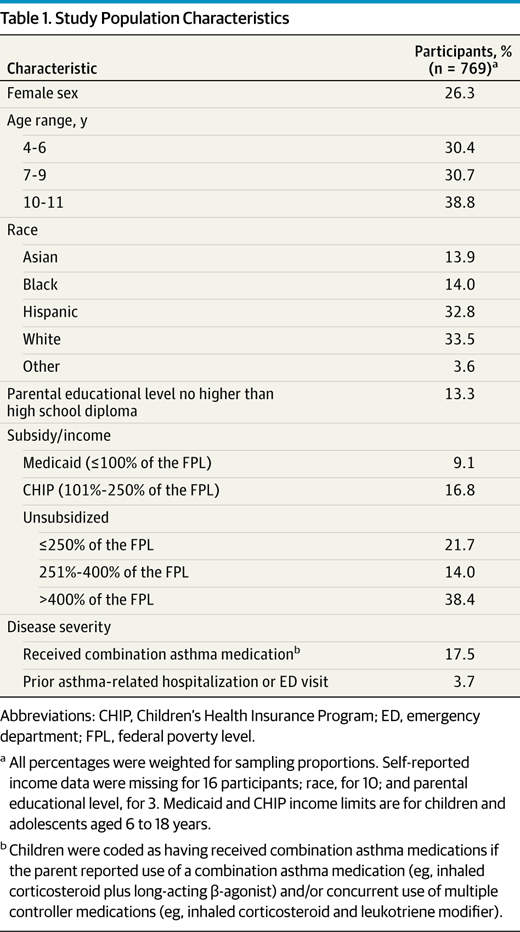
CHICAGO — According to a report published Monday by JAMA Pediatrics, cost-related barriers to care among children with asthma are concentrated among low-income families with higher cost-sharing levels. And while the Affordable Care Act’s low-income subsidies may reduce these barriers for many families, millions of dependents for whom employer-sponsored family coverage is unaffordable could remain at risk for cost-related problems because of ACA subsidy eligibility rules, the report concluded.
Overall, 15.6% of parents borrowed money or cut back on necessities to pay for their children’s asthma care, the report noted.
After adjustment, parents at or below 250% of the federal poverty level with lower vs. higher cost-sharing levels were less likely to delay or avoid taking their children to a physician’s office visit (3.8% vs 31.6%) and the emergency department (1.2% vs 19.4%) because of cost. Higher-income parents and those whose children were receiving public subsidies (e.g., Medicaid, CHIP) also were less likely to forego their children’s care than parents at or below 250% of the FPL with higher cost-sharing levels.
"We found that delaying and avoiding health care because of costs was concentrated among commercially insured children with higher levels of cost sharing and household incomes at or less than 250% of the FPL," researchers noted. "The ACA will expand cost-sharing subsidies to families with incomes at or below 250% of the FPL, which could reduce cost-related barriers to care, especially for families with children with chronic conditions like asthma and living in states with lower income eligibility limits for CHIP. For families at 200% to 250% of the FPL, however, these cost-sharing subsidies will be modest," they added. "Moreover, because of a family glitch, these subsidies will not be available to millions of dependents for whom employer-sponsored family coverage could be unaffordable. Work is needed to evaluate the effects of the ACA and potential unintended gaps in subsidy access to inform ongoing policy refinements."
Studies examining the effects of expanding subsidized coverage to poor children, such as through Medicaid or CHIP, have found improvements in access to care. According to the researchers, one recent study of commercially insured children with asthma found that higher cost-sharing for drugs was associated with modest reductions in the use of medication and increases in asthma-related hospitalizations for older children. However, limited evidence exists on responses to cost sharing for care other than drugs and on variations across income levels to inform low-income subsidies mandated by the ACA.