Pharmacy’s battle for provider status reaches crescendo at state, federal level
“All providers in the healthcare system should practice to the fullest extent allowed by their license.”
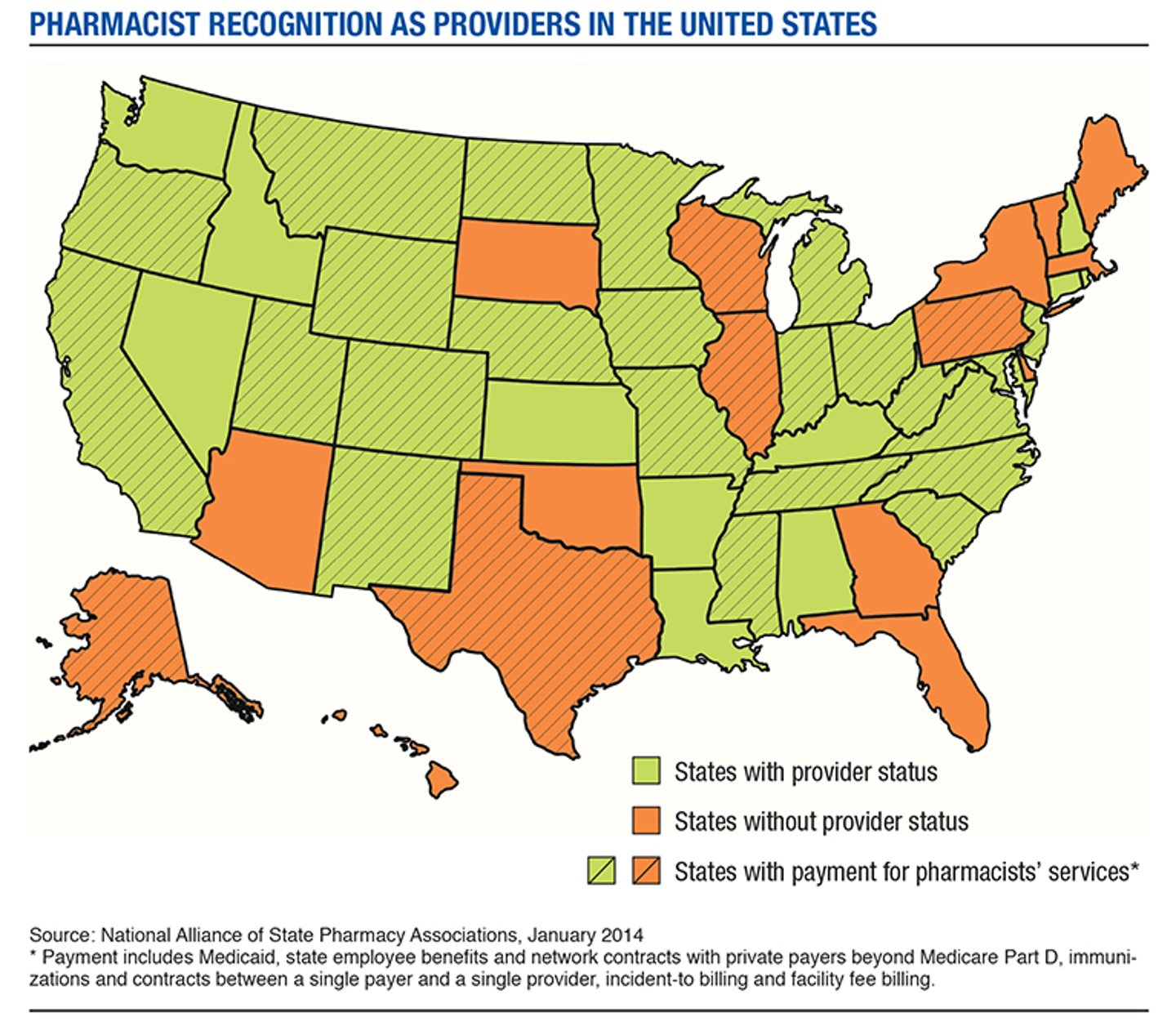
That principle, espoused by a national coalition of pharmacy interest groups working fervently to achieve provider status and recognition for pharmacists, seems straightforward enough. But gaining full provider status — and the fair reimbursement for pharmacy care services that would come if government and private health plan payers included pharmacists in the federal and state definition of a healthcare provider — continues to elude the profession.
The ongoing debate over pharmacists’ value and contribution to better health outcomes persists in the face of clear evidence that “community pharmacy can play an important role in helping to prevent and treat acute and chronic conditions,” said Kermit Crawford, Walgreens president of pharmacy, health and wellness. Earlier this month, Crawford announced his retirement from Walgreens at the end of the year.
“With new patients entering the system, a primary care physician shortage, an aging population and a growing prevalence of chronic diseases, there is a great need for convenient access to quality health care services,” Crawford said.
Pharmacy’s battle over recognition also lingers despite the fact that many health professionals other than physicians have provider status under Medicare Part B, the American Society of Health-System Pharmacists reported. The list includes physician assistants, nurse practitioners, clinical nurse specialists, certified registered nurse anesthetists, certified nurse-midwives, clinical social workers, clinical psychologists and registered dietitians or nutrition professionals, ASHP noted.
Nevertheless, “pharmacists are not currently recognized as healthcare providers under federal law, despite having more medication education and training than any other health care professional,” noted Tom Menighan, EVP and CEO of the American Pharmacists Association. “Beyond being unfair to our profession, this lack of federal recognition restricts the contributions pharmacists can make to improving patient care.”
Achieving recognition as designated health providers by Medicare, Medicaid and for-profit managed care plans would mean that “pharmacists are compensated directly by a third-party payer for providing medication therapy management” and other patient care services, noted ASHP. So the lack of provider status also hits community pharmacy hard in the pocketbook. Without that professional recognition, the industry is locked in a perpetual struggle with health plan payers to establish commonly accepted payment standards for medication therapy management, advanced counseling, and disease monitoring and man agement for patients with chronic conditions, among other services.
This is the case despite a growing mountain of evidence showing the cost-saving value to managed health plans and plan payers of pharmacist interventions and collaborative care models that incorporate pharmacists in a team-based approach to patient care. “The evidence shows that when pharmacists are included in medication management, costs go down and quality improves,” Menighan said.
Simply put, “patients’ access to pharmacist-provided patient care is critical to ensuring optimal health outcomes and efficient healthcare delivery,” declared Rebecca Snead, EVP and CEO of the National Alliance of State Pharmacy Associations, one of the organizations on the forefront of the campaign for provider status.
“If spending and outcomes are to be optimized, benefits and healthcare systems must include pharmacist services in collaboration with other providers,” said Lawrence Brown, associate dean and professor of pharmacoeco-nomics and health policy for Chapman University School of Pharmacy.
“When pharmacists are involved, costs go down and quality improves,” Brown declared in a presentation to the Illinois Pharmacists Association last fall. “Provider status for pharmacists will result in a team-based, patient-centered healthcare system, providing improved care and value.”
The absence of uniform payment standards — and the continuing resistance to adopting any reimbursement standard for pharmacists by many health plans and payers — presents pharmacy with one of its toughest fundamental challenges going forward. It undercuts the profession’s evolution beyond drug dispensing and basic counseling, and threatens the in-dustry’s future as a viable, sustainable business model, as margins continue to contract for prescription dispensing and the health payment system shifts inexorably to evidence-based reimbursements and accountable care.

Chipping away at federal, state barriers
The battle for full professional recognition has been taken up by virtually every pharmacy advocacy group, including APhA, NASPA, the National Association of Chain Drug Stores, the National Community Pharmacists Association, ASHP and the Food Marketing Institute. In turn, it’s spawned the formation of ad hoc coalitions like Patient Access to Pharmacists’ Care Coalition, whose purpose is to persuade federal and state legislators and regulators to pass laws and regulations that would grant full provider status to pharmacists.
“A campaign to advance pharmacist provider status ... addresses one of the most critical issues for our profession and remains APhA’s primary focus,” APhA’s Monighan reported. “This is a long-term, strategic effort that must be pursued vigorously if patients are to use their medicines successfully, and if our profession is to be relevant in an evolving healthcare system.
“That’s why APhA has embarked on a campaign to achieve provider status, which will recognize pharmacists as valued members of the healthcare team, and allow us to use our unique skills and extensive education to enhance patient health,” he said.
Through coalitions like PAPCC, the industry is working across a broad front to educate lawmakers at the federal and state level and promote new legislation and regulations aimed at gaining full provider status. The outreach campaign extends to Congress, state legislatures, the Federal Trade Commission and the U.S. Centers for Medicare and Medicaid Services.
One key goal: to “promote and facilitate pharmacist registration for National Provider Identifier numbers,” according to a report from the Florida Pharmacy Association and Kayla Mackanin, a PharmD candidate from the University of South Florida.
“The NPI number is the CMS HIPAA standard for identifying healthcare providers,” Mackanin reported. “In order to submit claims to ... CMS for services provided to patients, recognized health providers must have and use their NPI.”
Thus, wrote Mackanin, “pharmacist inclusion in the CMS definition [for health providers] is key. CMS recognition will remove current limitations on the type of services and amount of reimbursement pharmacists are eligible for when submitting claims to CMS.”
PAPCC and other groups also have focused their lobbying effort on the FTC, urging federal antitrust regulators focused on healthcare competition to back legislation “that would help pha